Transcutaneous Ablation of Septal Hypertrophy
Treatments for HOCM include medication to control the heart’s contraction, insertion of pacemakers to prevent arrhythmias, and — when medications fail — surgical resection of the thickened septum, making it thinner. Dr Aroney at Holy Spirit Northside Hospital offers alcohol septal ablation as an alternative to surgery in selected patients. He performed the first such procedure in Australia in 2000, and has performed the largest numbers of this procedure in Queensland.
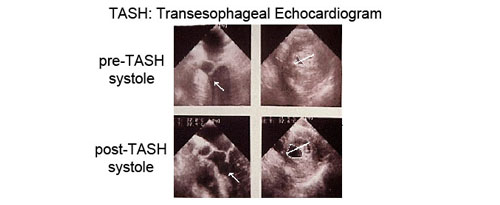
This treatment for HOCM actually reduces the obstruction and improves blood flow out of the heart. In addition, it often improves the function of the mitral valve. During alcohol septal ablation, a balloon catheter is inserted in the groin and is led to the heart. Echocardiographic contrast material is first injected to ensure proper localisation and then a small amount of pure alcohol is introduced into the vessel. This results in carefully controlled damage to that part of the abnormally thickened septum. A thinner wall of scar tissue that reduces the obstruction and improves the overall function of the heart will replace the septum. Many patients feel immediate improvement of their symptoms; the majority continue to improve over many months.
Description of the procedure:
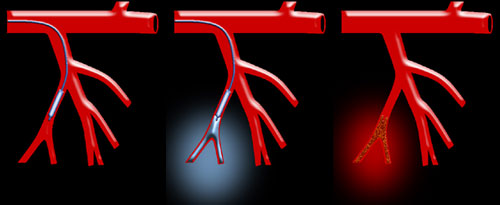
This procedure involves injecting 100% absolute alcohol into one of the branches of a heart artery that feeds the enlarged septum. The alcohol occludes the septal artery, and is very toxic to the heart muscle cells, and causes it to die and shrink. The thickened heart muscle is replaced with thin scar tissue, and thus the obstruction to blood flow out of the left ventricle is reduced. This procedure is performed in the cardiac catheterization lab. On the day of the procedure, an informed consent is obtained from the patient. A baseline ECG is performed. Blood is collected for cardiac markers before, during and after the procedure. Medications will be given at this time to relax the patient and reduce the pain. The cardiologist will then insert 2 tubes (sheath) into the artery and the vein in the patient’s groin or neck. A temporary pace maker will be passed through the venous sheath and advanced into the right ventricle of the heart. Baseline echocardiography will be performed and repeated during the procedure.
Coronary angiography is then performed, so the cardiologist can localize the origin of the septal arteries. A balloon-tipped catheter will be threaded over a wire and guided into a branch of the artery that provides blood supply to the enlarged septum. Once in place, the balloon catheter will be inflated to block the artery, and 3-5 cc alcohol will be injected at approximately1cc/min. The balloon will be deflated and removed after 5 minutes. The patient remains awake throughout the procedure, and may feel chest discomfort when the alcohol is being injected but pain medications will be administered if needed. Angiography will be performed afterwards to confirm the occlusion of the target septal artery branch. Pressure gradients within the left ventricle is then measured by inserting a catheter into the left ventricle. The temporary pacemaker is sutured in place. The Patients will be transferred to the coronary care unit for close monitoring. The pacemaker lead will be removed the next day. If there are no complications, patients will be discharged after 2-3-nights.
The most common side effect of this procedure is an electrical conduction abnormality called “complete heart block” which requires permanent pacemaker implantation. This complication has been reported to occur in up to 15% of treated patients. Other potential complications include heart attack in the non-target territory, irregular heart rhythm, bleeding, infection, allergic reaction to the dye, kidney failure from the dye, perforation of the artery, dissection of the artery, septal rupture and death. All of these complications are extremely rare.
It is important to know that not all HOCM patients are good candidates for this procedure. The cardiologist will evaluate and determine whether a patient meets all the criteria to undergo alcohol ablation.
If you have any further questions, please contact us at:
Queensland Cardiology
St Vincent’s Private Hospital Northside
North Medical Suites, Green Lifts Level 3,
627 Rode Road
Chermside Q 4032
(07) 3861 5522